by Sleep Better Columbus | May 25, 2020 | Sleep Apnea
Sleep apnea is a sleep disorder viewed by many as something minor and not much to worry about. But when you look beneath the surface and ask what does sleep apnea cause, astonishing details are revealed. As a result, in the past few years, this myth has been busted. And sleep apnea has become a widely popular topic. Why? Because of what life-threatening diseases it can cause or worsen.
However, there is so much more work to be done in spreading the word. In this article, we are going to go over some of the disorders that can manifest because of sleep apnea and how ignoring the signs and symptoms can cause more harm. You will learn how to recognize these symptoms and what you can do to get treated.
Sound good? Great… Let’s get started.
Sleep Apnea and Common Disorders It Can Cause
There are over 800 sleep disorders, but sleep apnea is the one more common in the United States. And has become a significant reason for health issues. It’s been confirmed that over 22 million Americans grapple with sleep apnea every night.
About 1 out of every 12 Americans suffer and are inadvertently encouraging future healthcare complications because of sleep apnea when it’s left undiagnosed and treated. And sadly, undiagnosed sleep apnea is the truth for 80% of cases.
So how do you avoid falling victim to perpetual healthcare decline from sleep apnea? You do so, by becoming aware and following the steps to get diagnosed and then treated by a sleep study doctor such Dr. Levy of Sleep Better Columbus. After all, if you suffer from sleep apnea you want someone who can improve your quality of life quickly and make things comfortable for you.
Common Disorders Sleep Apnea Promotes
Asking what does sleep apnea cause, but the greatest minds in sleep medicine to work. It’s only when the right questions are asked that the solution of the best treatment for a problem gets solved. Here is a list of the most common diseases affiliated with sleep apnea.
- High Blood Pressure (hypertension)
- Chronic Heart Failure (CHF)
- Atrial Fibrillation (AFib)
- Stroke (loss of blood flow to the brain)
- Depression
- Type-2 Diabetes
- Liver Problems
- Excessive Day Time Fatigue
As you can see, the list above is filled with serious life-threatening conditions and can cause life long consequences if discovered too late.
For example, how much would your life change if you fell asleep at the wheel? Or you drifted off to sleep as you were cooking something on the stove? These mistakes happen every single day because of sleep apnea. If you experienced either one these, how would your life be different?
Worsening Disorders
When you are already suffering from a disease or disorder like chronic heart failure obstructive sleep apnea will make it significantly worse. See when you fail to breathe as you sleep, you cause your co2 (aka) carbon monoxide to build up in your blood. As you breathe regularly moving oxygen and co2 in and out of your body you naturally retain some co2. But people who have sleep apnea have less oxygen in their blood and higher co2 levels.
This creates your blood to become thicker and also stunt the receptors in your body that tell your brain to breathe when sleeping. This causes more stress on the heart to work harder and harder, attempting to bring back homeostasis. Unfortunately without treatment of your sleep apnea, you remain in a vicious cycle of deterioration.
The only way to fix it is with help from a sleep doctor who can properly treat your individual case with the right positive pressure treatment or oral appliance treatment. It all depends on your type of sleep apnea.
This is only one case study of a worsening disorder. There are several outcomes base on the disease that sleep apnea can worsen.
Common Risk Factors To Sleep Apnea
Gender – Middle-aged and older men are more likely to acquire sleep apnea. Sleeping disorder breathing affects almost 50% of men and only 24% of women.
Note: Smoking drastically increases the risk of sleep apnea regardless of gender.
Obesity – There is a relationship between sleep apnea and obesity in around 60% of the cases that are diagnosed. Having a thicker neck because of larger fat deposits will instantly cause an increased risk of obstructing your airway.
Narrow airway – Conversely, being born with or having been in an accident that decreases your airway circumference, will also increase your risk for OSA.
Substance abuse – Using any sedatives or narcotics that impair the nervous system will increase your chances of sleep apnea, more so for CSA (Central Sleep Apnea). You must be careful when taking medications prescribed and know how your body will react.
Stroke – As we mentioned earlier, sleep apnea can cause a stroke. However, if you have already suffered from a stroke you are at a higher risk of acquiring this chronic disorder.
Having a family history – At times you will be predisposed to sleep apnea because it runs in your family. This doesn’t mean you’re destined for sleep apnea, it only means you must be vigilant in your awareness of how you are feeling. And paying attention to the symptoms of sleep apnea presents.
Knowing what sleep apnea causes is part of the puzzle when piecing together the treatment and management of sleep apnea. Knowing how to pay attention to how you feel is also important. Here are some of the most common symptoms you can look out for – in your behavior or those close to you.
- Snoring loudly
- Chronic morning headaches
- Waking up in the middle of the night gasping for air
- Holding your breath in your sleep (observed by someone else)
- Lack of focus while awake
- Irritable
- Insomnia (or waking up multiple times throughout the night)
- When you wake up you have extremely dry mouth
- Exhaustion throughout the day
These are some common symptoms of sleep apnea. And ones to pay attention too for signs you may need to see a sleep study specialist like Dr. Levy from Sleep Better Columbus.
In Conclusion
By now we don’t have to convince you that your sleep health is a necessity for a safe and happy life. Dr. Levy has treated hundreds of patients suffering from sleep apnea. He uses sleep study methods that help diagnose your sleep apnea is a comfortable way. Then afterward sit’s down with you and discuss your best options on treatment.
You may need an affordable state of the art CPAP device, or you may decide to use an oral appliance. You see, with the oral appliance you are fitted for a mouthpiece that can make sleep apnea treatment a breeze. Let our professional team help you with your diagnosis and treatment to ensure you live a long and healthy life.
It’s no longer hard to be diagnosed and treated. You’re not alone. Take the knowledge and the awareness of sleep apnea and make sure you avoid the mistakes so many others fail to avoid. Dr. Levy and staff at Sleep Better Columbus welcome you to call us at (614) 362-7292. The answer to the question – what does sleep apnea cause? Has been answered. The only thing left for you to do is trust us to help.

by Sleep Better Columbus | Apr 9, 2020 | Sleep Apnea
A new study conducted by the Brigham and Women’s Hospital in Boston suggests that irregular sleep patterns may double your risk of heart disease. “Our study indicates that healthy sleep isn’t just about quantity but also about variability, and that this can have an important effect on heart health,” says Huang, the lead author on the study.
What Is Heart Disease?
Heart disease describes conditions that affect how the heart functions. It can refer to heart defects or conditions that cause irregular heart beats. These diseases can also affect the tissues surrounding the heart, such as the blood vessels and arteries. Heart disease includes the following conditions:
- Congenital Defects
- Arrhythmia
- Coronary Artery Disease
- Dilated Cardiomyopathy
- Myocardial Infarction (Heart Attack)
- Heart Failure
- Hypertrophic Cardiomyopathy
- Mitral Regurgitation
- Mitral Valve Prolapse
- Pulmonary Stenosis
According to the Center for Disease Control, “Heart disease is the leading cause of death for men, women, and people of most racial and ethnic groups in the United States.” This translates into heart disease being the leading cause in 1 of every 4 deaths in the US.
Risk Factors
High blood pressure, high cholesterol, and smoking are major risk factors for heart disease. According to the CDC, roughly half of Americans (47%) have at least one of these risk factors. Other health issues and lifestyle choices also increase your risk. These factors for heart disease include:
- Age – Age increases your risk of a variety of health problems. As we age the tissues of the heart and arteries thicken, become weak, or simply break down over time.
- Sex – Men are at increased risk of developing heart disease. Doctors believe this is due to where men carry most of their weight. A woman’s risk of heart disease increases after menopause.
- Family History – Your genes may predispose you to developing certain types of heart disease. Your risk may be especially high if a parent developed heart disease at an earlier age than normal.
- Diet – Diets high in fats, sugar, salt, and cholesterol can contribute to heart disease.
- Diabetes – Diabetes shares many of the same risk factors as heart disease.
- Obesity – Excessive weight gain worsens many of the other risk factors for heart disease.
- Physical Inactivity – Less active, less fit individuals are more likely to develop high blood pressure. They are also more likely to develop diabetes and become obese.
- Stress – Stress damages your arteries and worsens other risk factors.
These risk factors are well documented by decades of studies and research. However, one major risk factor that has gone largely unresearched until now is sleep. “When we talk about interventions to prevent heart attacks and stroke, we focus on diet and exercise,” says Huang. “Even when we talk about sleep, we tend to focus on duration – how many hours a person sleeps each night – but not on sleep irregularity and the impact of going to bed at different times or sleeping different amounts from night to night.”
What we have learned from these decades of sleep studies is that sleep duration is very much a ‘Goldilocks’ zone. If you are getting too much or too little, your health outcomes decline. But when your amount of sleep is ‘just right’ health outcomes improve. These studies show that too much sleep has many of the same negative effects as too little sleep. And both contribute dramatically to many of the same risk factors for heart disease. According to a Gallup poll, the typical American adult gets less than 7 hours of sleep a night. While individual sleep needs may vary slightly, most people perform best on 8 hours of sleep a night. But if the duration of sleep was the only factor, then those who get 8 hours each night should have a lower risk, right? The study found that it may not be that simple.
The Brigham and Women’s Hospital study found that variation in bedtime and sleep duration had a major impact on health outcomes. The data showed those whose bed time varied by 90 minutes or more, and whose sleep duration varied by 2 or more hours a night were at the greatest risk. This group was “more likely to develop metabolic disorders such as hypertension, obesity and diabetes.” As a result, this group also reported nearly double the number of heart problems and cardiovascular events.
How Do I Reduce My Risks?
Huang states that “Sleep regularity is a modifiable behavior. In the future, we’d like to explore whether changing one’s sleep patterns by going to bed consistently each night may reduce a person’s risk of future cardiovascular events.” There are many things you can do to ensure a more consistent bedtime, including the following:
- Have a set bedtime
- Don’t wait to feel sleepy before getting ready for bed
- Turn off your phone, computer, and TV an hour before bed
- Avoid caffeine
- Have a nightly routine
Altering your habits to ensure a consistent bedtime and sleep duration should help reduce your risks.
Could Sleep Apnea Be To Blame?
The study did not address the causes of irregular sleep patterns, but they hypothesized that frequent waking was a factor. As many as 70 million US adults suffer from a some form of sleep disorder. The most common of which is Sleep Apnea.
Around 1 in 5 adults suffer from mild symptoms of Obstructive Sleep Apnea, with 1 in 15 having moderate to severe symptoms. Untreated, sleep apnea contributes to many of the same risk factors for heart disease. Unfortunately, most people who have the condition are unaware that they do. Researchers estimate that only about 20% of cases are ever diagnosed. If you have many of the same risk factors for heart disease or suspect you may not be getting restful sleep, speak with your doctor about sleep apnea.
Thankfully, sleep apnea is easy to treat. The usual, go-to treatment is to use a CPAP machine. With Obstructive Sleep Apnea the airway becomes partially or completely obstructed, preventing the movement of air through the lungs. The most common cause of obstruction is soft palate collapse. The soft tissues of the throat relax too much, blocking the airway. A CPAP works by pumping pressurized air into the airway to prevent airway collapse. However, CPAP masks are large, heavy, and often uncomfortable. As a result, patients often report low compliance with their prescribed sleep apnea therapy.
An equally effective, and less restrictive option is an oral appliance. An oral appliance is a device designed to fit in the mouth. It shifts the lower jaw forward to prevent soft palate collapse. At Sleep Better Columbus we know the importance of getting a good night’s sleep. And an uncomfortable heavy mask is not the best solution for most patients. We specialize in custom fitted oral appliances. We ensure you get the best fit for a better night’s sleep.

by Sleep Better Columbus | Mar 19, 2020 | Sleep Apnea
Sleep apnea can lead to many other health issues. Some of these health problems can cause sleep apnea, and others result from it. Interestingly, many of these health conditions involve the heart and lungs. So it might have you wondering: Can sleep apnea cause lung problems?
It’s true that sleep apnea affects your breathing. These apneas, or periods when breathing stops and starts, might make you think it is a lung disease. According to the American Lung Association, the term lung disease refers to any disorder affecting the lungs. This includes disorders like asthma, COPD, cancer, influenza, pneumonia, tuberculosis, and many others. While sleep apnea can have serious consequences for lung health, the primary function of the condition is sleep related.
What Is Sleep Apnea?
Before we look at how it affects your lung health, let’s look at what sleep apnea is.
Apnea is a ‘temporary cessation of breathing, especially during sleep’. Based on the definition, referring to the condition as ‘sleep apnea’ may seem redundant. But because apneas can occur at other times, it is an important distinction to make.
With sleep apnea, breathing stops and starts at least 5 times an hour, but can pause as many as several hundred times a night. These pauses can last anywhere from 5 seconds to several minutes at a time. When this happens, blood oxygen levels drop and trigger you to wake up. Frequent sleep disruptions causes a variety of side effects. These side effects may include:
- Irritability
- Slowed reaction time
- Difficulty focusing
- Fatigue
- Forgetfulness
- Driving accidents
- Depression
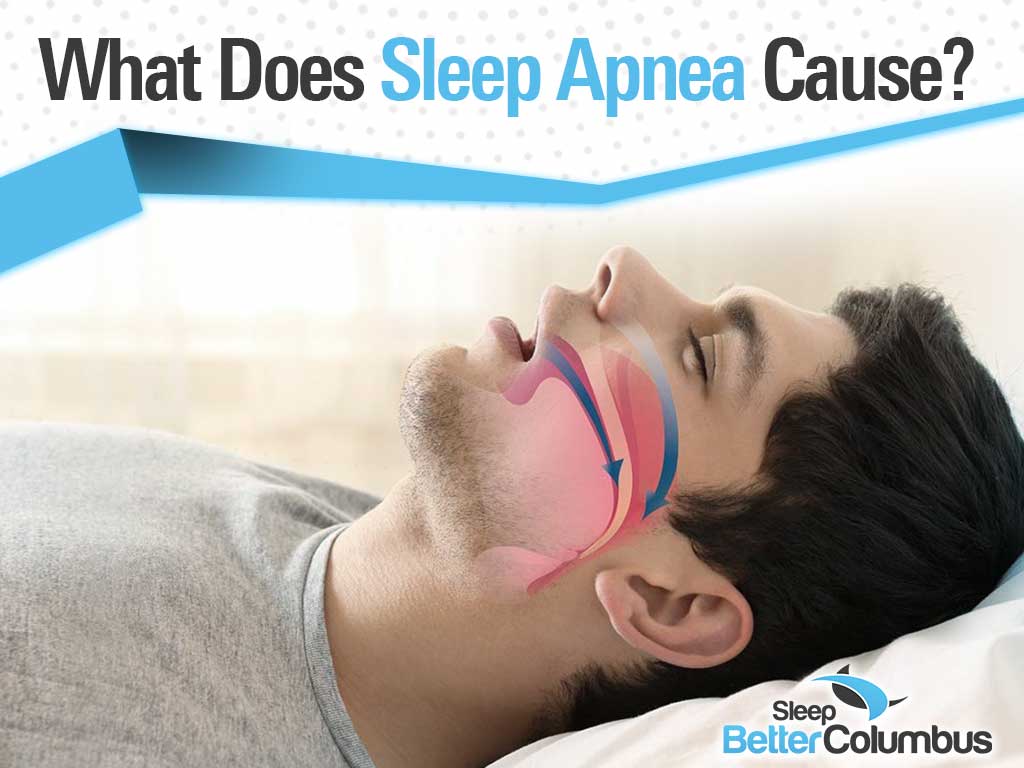
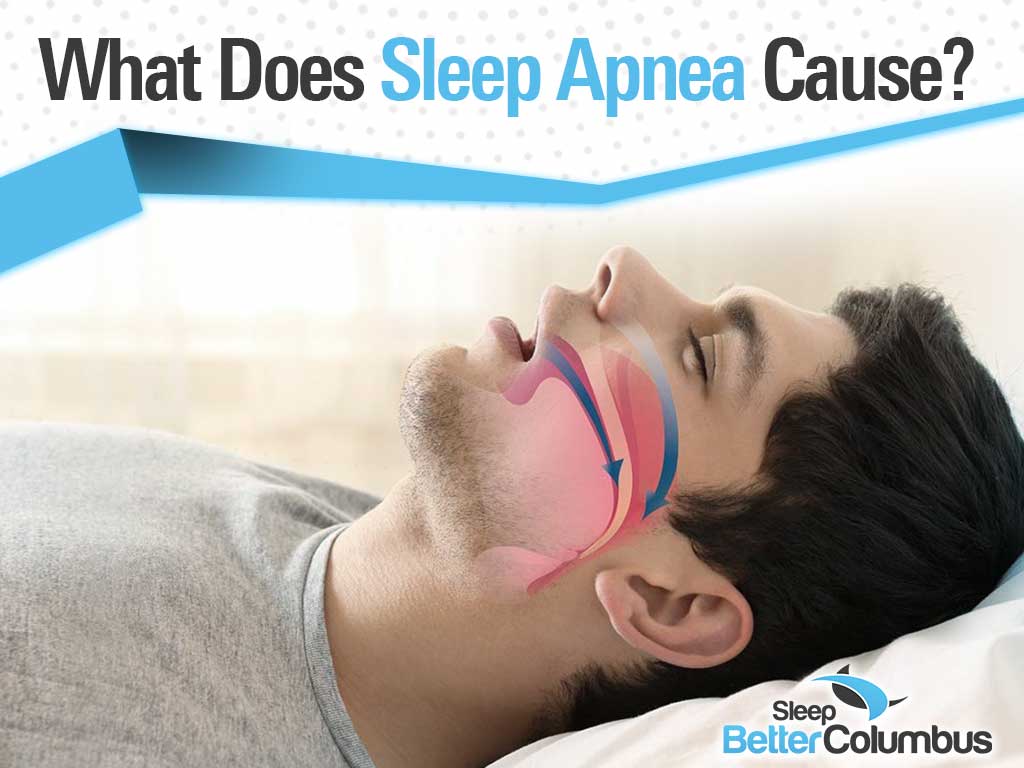
There are a few types of sleep apnea but the most common type is Obstructive Sleep Apnea (OSA). With OSA these apnea events occur when the airway becomes partially or completely blocked during sleep. The blockage may be due to several different factors.
Common causes of Obstructive Sleep Apnea are:
- Relaxation of the neck and throat muscles, causing the soft palate to collapse
- Tongue balling up in the back of the throat
- Fatty deposits in the tongue or neck restrict the airway
- Narrow airway
With OSA the brain continues sending messages to the body to breathe. The muscles of the chest and diaphragm work even harder to breathe but are not able to completely clear the blockage. This results in the loud snoring, choking, or gasping during sleep that is common for people with the condition.
Is Sleep Apnea a Respiratory Disorder?
With lung diseases the primary function of the disorder begins in the lungs. But, in sleep apnea the issue starts in the brain or in the airway itself and occurs only during sleep. As a result, it is most accurate to refer to sleep apnea as a form of sleep-disordered breathing.
Can Sleep Apnea Cause Lung Problems?
While classified as a sleep disorder, sleep apnea does lead to or worsen lung problems.
Research published in BMC Pulmonary Medicine found that patients with OSA had increased lung elasticity recoil pressure. The elastic quality of lung tissues is what allows them to expand and contract when you breathe. With increased lung elasticity recoil pressure the lungs snap back too forcefully. This creates a vacuum effect that contributes to airway collapse in OSA. The resulting reduction in lung volume increases the risk or worsens the symptoms of some very serious lung problems.
Lung problems that are common in patients with sleep apnea include:
- Chronic Obstructive Pulmonary Disease (COPD)
- Pulmonary Hypertension
- Asthma
COPD
Chronic Obstructive Pulmonary Disease, or COPD, is an umbrella term for a group of conditions that make breathing difficult. This difficulty arises from clogged or narrow airways. It is usually the result of inflammation in the internal structures or damage to the air sacs in the lungs. This damage is typically caused by smoking and air pollutants.
A review in the journal Lung found that up to 66% of COPD sufferers also suffer from sleep apnea. As where only around 20% of patients with sleep apnea also have COPD. Doctors refer to this as “overlap syndrome”. Patients with COPD have an increased risk of heart attack. When paired with sleep apnea it will lead to high blood pressure, arrhythmia, heart failure, and stroke if left untreated. Unfortunately there is no cure for COPD and the condition tends to worsen over time. However, symptoms do improve with treatment and the use of sleep apnea therapy .
Pulmonary Hypertension
Patients with sleep apnea have an increased risk of developing pulmonary hypertension (PH). Pulmonary hypertension is a type of high blood pressure. It causes increased blood pressure in the arteries of the lungs and in the right side of the heart. Patients with pulmonary hypertension experience shortness of breath, dizziness, and chest pressure. How exactly sleep apnea causes pulmonary hypertension remains controversial. However, we know that periods of low blood oxygen (hypoxia) cause the heart to work harder to continue supplying oxygen to the body. With sleep apnea these periods of hypoxia happen more frequently, sometimes several hundred times a night. Studies show that as many as 82% of patients with PH have some form of sleep apnea. Like COPD, pulmonary hypertension worsens over time. Similarly, patients can reduce the severity of their symptoms and improve quality of life with treatment.
Asthma
Asthma is a condition in which a person’s airways are highly sensitive. When exposed to a trigger the airway becomes inflamed and swollen, restricting the flow of air through the lungs. This irritation also causes the lungs to secrete more mucus, making it even harder to breathe. Asthma and sleep apnea are both common conditions and seem to play off each other. In the BCM Pulmonary Medicine review researchers found a synergistic link between the two conditions. Subjects with OSA had a narrower airway on average, as did subjects who only had asthma. Airway diameter was even smaller in subjects who had both. They found that 49% of subjects with difficult-to-treat asthma also suffered from mild to moderate OSA. The data also showed a direct link between how intense their OSA was and the severity of their asthma symptoms. When asthma is well controlled, OSA symptoms also decrease.
Reduce the Risk of Your Apnea and Lung Problems
The good news is that sleep apnea is easy to treat. Patients see improvement in their quality of life soon after beginning sleep apnea therapy . At Sleep Better Columbus we know how important it is to get a good night’s sleep. CPAP machines are a great option but we know they can be uncomfortable and make sleeping difficult. We provide high quality, custom fitted oral appliances to keep your airway clear. An oral appliance shifts the lower jaw forward. This prevents soft palate collapse and keeps the tongue from balling up at the back of the throat. Because our oral appliances are lightweight and custom fitted, patients have an easier time adjusting. This results in better compliance and faster relief. Reducing your symptoms will improve your quality of life and reduce your risks of lung problems.

by Sleep Better Columbus | Mar 12, 2020 | Sleep Apnea
Sleep apnea is a serious condition in which breathing stops and starts during sleep. These pauses in breathing last for at least 10 seconds at a time and occur no less than 5 times an hour. These pauses cause blood oxygen levels to drop, triggering periods of wakefulness. Unfortunately, symptoms of sleep apnea are easily missed or often ignored. Many patients are not aware of their condition until it has already taken a serious toll on their health. But what triggers sleep apnea?
Types of Sleep Apnea
Before we can dive into what triggers sleep apnea (SA), let’s take a look at the different types. There are two main types:
With central sleep apnea (CSA) the wiring in the brain has become faulty. The brain fails to properly send signals to the muscles that control your breathing. Unlike obstructive sleep apnea, in CSA all breathing functions stop. It is not until oxygen levels drop enough that the brain is able to trigger you to wake up abruptly. This form of sleep apnea is less common.
Obstructive sleep apnea (OSA) is by far the most common. It is the result of the soft tissues of the mouth and throat relaxing too much during sleep. These structures collapse inward, either partially or completely blocking the airway. During an episode of OSA the brain continues sending signals to breathe. With a partial obstruction the added effort causes the soft tissues to vibrate. This results in the loud, chainsaw-like snoring associated with OSA. A complete obstruction results in observable periods where breathing stops. Either type of episode usually ends with a fit of gasping or choking before normal breathing resumes.
While it is possible to have both forms of SA, it is not as common. Doctors refer to this as complex sleep apnea. Patients will have alternating periods of apnea due either to failed signals or obstruction.
What Causes Sleep Apnea?
There are many causes and contributing factors in sleep apnea. Central sleep apnea is the result of the brain failing to signal the muscles of the chest to breathe. Conditions that reduce blood oxygen levels or impair the function of the central nervous system can increase your risk. Factors that increase the risk of CSA include:
- Age – As you age your risk of developing CSA increases. The groups most at risk are individuals over the age of 45 are at the greatest risk.
- Biological Sex – CSA is more common among men than it is among women.
- Heart Health – Heart health can have a tremendous impact on your risk factors. Conditions such as congestive heart failure or an irregular heartbeat are significant risk factors for CSA.
- Medications – Certain medications, particularly sedatives, opioids, and methadone can increase your risk.
- Stroke – Around 75% of patients who need physical therapy after a stroke are also diagnosed with sleep-disordered breathing. CSA is the most common diagnosis.
- Other Brain Abnormalities – Brain tumors and lesions on the brain stem can impair its ability to properly relay messages to the body.
- CPAP Use – Studies show that patients who use a CPAP machine to create positive pressure in their airway are more likely to develop CSA. Continued use of a CPAP often resolves this issue.
Obstructive sleep apnea is most greatly influenced by physical factors. Factors that increase your risk of developing OSA include:
- Weight – Obesity and excessive weight greatly increases the risk of sleep apnea. Fat deposits in the tongue and neck can obstruct breathing.
- Narrow Airway – Some people naturally have a narrow airway. Others may have enlarged tonsils or adenoids. While this can be an issue in adults, it is often identified and addressed in childhood. Having a thick neck can also cause a narrowing of the airway.
- Biological Sex – As with CSA, obstructive sleep apnea is more common in men than in women. Men are as much as 3 times more likely to develop the condition. Men tend to put on more weight in their midsection than women. Increased abdominal circumference is directly linked to OSA. Women have an increased risk of OSA if they are overweight or are post-menopause.
- Age – OSA is more common in adults over the age of 40.
- Family History – Many risk factors for OSA are hereditary.
- Substance and Drug Use – Alcohol, sedatives, and tranquilizers relax the muscles of the throat and slow your breathing.
- Smoking – Smoking causes inflammation and fluid retention in the upper respiratory tract. This narrows the airway and increases a smokers risk three times more than people who have never smoked.
- Nasal Congestion – Swelling in the nasal passages can cause the airway to become blocked or narrowed, especially when lying down. This may be due to allergies or illness. Anatomical abnormalities such as a deviated septum can also compound this issue.
Reducing Your Risks
Some risk factors like age, biological sex, and heredity are beyond your control. Some may require surgical correction. But, through an appropriate treatment plan you can reduce many other risk factors.
Ways you can reduce your risks include:
- Weight Management – Doctors recommend that most patients with sleep apnea lose weight. Maintaining a healthy weight can reduce many key risk factors.
- Exercise – A moderate exercise routine can strengthen your heart and improve circulation. Regular exercise can also improve lung capacity. This helps to reduce how often you wake due to poor oxygenation.
- Reduce Medication and Drug Use – Reducing the use of opioids, sedatives, and tranquilizers will lower your risks.
- Avoid Smoking and Drinking – Quitting smoking is a great way to reduce your sleep apnea risk factors. As your lungs recover, airway irritation will reduce and allow for clearer breathing. Avoiding alcohol use before bed, or cutting it out altogether will also help.
- Humidifier – Some airway obstruction is the result of inflammation. Using a humidifier helps to sooth and open the airway for clearer breathing.
- Sleep Position – Depending on the cause of your obstruction, changing your sleep position may provide relief. Studies show that adults with OSA may benefit from side sleeping. Oddly, the same is not true of children with OSA. The same study showed that back sleeping reduces symptoms in children.
- Oral Appliances – An oral appliance is a mouthpiece very similar in design to a sport mouthguard. This custom fitted mouthpiece helps to angle the jaw and tongue forward to prevent soft palate collapse. Patients report faster relief from symptoms and a better rate of compliance than with a CPAP.
It is important to take a combined approach to sleep apnea relief. Addressing underlying health issues and reducing risk factors will improve your quality of life. In the meantime, you need to get restful sleep. At Sleep Better Columbus we know the fastest, safest way to help you find relief is to use a custom oral appliance. Dr. Mark Levy has used oral appliance therapy to treat sleep apnea since 2005. He has dedicated himself to continuing his education to provide patients with the best possible care. At Sleep Better Columbus you can be sure you’ll get excellent care, quality appliances, and better sleep.
by Sleep Better Columbus | Mar 5, 2020 | Sleep Apnea
Sleep apnea is a common sleep disorder affecting an estimated 42 million Americans, affecting roughly 1 in 5 adults. Approximately 9% of middle aged women and nearly 25% of middle aged men suffer from some form of sleep apnea. Disturbingly enough, however, most people who have sleep apnea are not aware that they do. Estimates suggest that as many as 75% of severe cases of sleep-disordered breathing go undiagnosed. Sleep apnea is also a major risk factor for serious life-shortening cardiovascular and metabolic health issues. But what is it and what makes sleep apnea so dangerous?
What Is Sleep Apnea?
Sleep apnea is a condition where a your breathing pauses for at least 10 seconds during sleep. In some cases these episodes may last several minutes before normal breathing resumes. The average healthy adult may have up to 5 episodes of paused breathing an hour during sleep. This is fairly normal and typically nothing to be concerned with. However, with sleep apnea these episodes occur at least 5 or more times an hour. In extreme cases a sufferer may have as many as 240+ episodes during an 8 hour night.
There are three types of sleep apnea. Obstructive sleep apnea occurs when the airway becomes blocked. This blockage either reduces or completely stops the flow of air through the lungs. During these episodes the body continues to try to breathe. The muscles of the chest and diaphragm work harder to try to force the airway open but are not able to. The most common cause of obstruction is the muscles of the neck and throat relaxing too much. As a result, the airway collapses. This obstruction reduces the flow of oxygen to your brain. When levels drop too low it triggers the gasp reflex, reopening your airway. Obstructive sleep apnea is the most common form of sleep apnea.
Central sleep apnea occurs when the brain fails to send proper signals to the body. Normally, breathing is an involuntary action. You keep on doing it whether you consciously choose to or not. But sometimes these signals fail to send due to differences in brain function. In this case, the airway is not blocked but there is no movement of air through the lungs. Breathing resumes when the oxygen levels drop low enough to trigger the gasp reflex. Central sleep apnea is less common but is, perhaps, the most dangerous form of apnea. It is possible to have both forms.
Signs of Sleep Apnea
One of the most interesting things about sleep apnea is that most people who have it are not even aware that they do. Diagnosis usually only comes after prolonged complaints from the patient’s sleep partner. Due to the nature of the condition misdiagnosis is common. Many doctors believe that sleep apnea is commonly misdiagnosed as depression, explaining why many cases of depression fail to respond to typical treatment. It is also common for patients to ignore their symptoms, writing it off as something else.
- Excessive daytime sleepiness
- Loud snoring
- Observable episodes of paused breathing during sleep
- Waking suddenly, usually accompanied by gasping or choking
- Morning dry mouth or sore throat
- Morning headache
- Difficulty concentrating during the day
- Changes in mood, such as depression or irritability
- High blood pressure
- Nighttime sweating
- Decreased libido
Not all sufferers experience every one of these symptoms. In fact, some individuals with sleep apnea do not snore at all.
Complications of Sleep Apnea
Because the symptoms of sleep apnea are easily missed and often go unnoticed by sufferers, it might lead you to wonder: Is sleep apnea dangerous? In a word, yes. While not typically immediately fatal, sleep apnea is caused by or contributes to many serious health issues. Interestingly, many of the risk factors that contribute to sleep apnea may also result from apnea itself. People most at risk of developing sleep apnea have one or more of the following traits:
- Male
- Obesity (BMI >30)
- Hypertension
- Alcohol or sedative use
- Abnormalities in airway or facial structure
- Smoker
- Family history of sleep apnea
- Large neck circumference
- Type 2 diabetes
- Metabolic disorder
Studies also show that patients with sleep apnea have a dramatically higher risk of developing the following:
- Hypertension, especially drug-resistant
- Obesity
- Congestive Heart Failure
- Need a pacemaker
- Atrial Fibrillation
- Diabetes
- Coronary Artery Disease
- Stroke
Studies have shown that sleep apnea is an independent risk factor for hypertension. Patients with no other risk factors are more likely to develop hypertension if they have sleep apnea. Sleep apnea also contributes greatly to stroke. Some 65-70% of stroke patients are also diagnosed with sleep-disordered breathing.
Sleep apnea was also found to double your risk of traffic accidents. The risk is significantly higher in people with moderate to severe sleep apnea. These individuals are 15 times more likely to cause an accident. This is due to excessive sleepiness and difficulty concentrating reducing reaction times. Estimates show that sleep apnea contributes to 980 traffic accident deaths per year.
Treating Sleep Apnea
Thankfully, sleep apnea is easy to diagnose and to treat, including treating sleep apnea effectively. If you suspect you may have sleep apnea, the first thing to do is speak with your doctor. Before your appointment, be sure to keep a sleep diary. Record how often you wake in the night and any other symptoms you have noticed. Have your sleep partner record how many times they notice you waking or stopping breathing in the night. This information will help your doctor to diagnose your condition. Your doctor will either give you a home test kit, or schedule a sleep study. The data collected during your test will show how often your breathing pauses, for how long, and how much your oxygen levels dip. With this information your doctor will be able to diagnose what form of sleep apnea you have and how to treat it.
Long term treatment for sleep apnea involves reducing your risk factors. This may include losing weight, lowering your blood pressure, and ensuring your diabetes is well controlled. Reducing or eliminating alcohol or sedative use will also reduce your risk. Unfortunately, it may not be possible to completely eliminate your risk factors.
More immediate solutions for treating sleep apnea involve the use of assistive devices.
- CPAP – Continuous Positive Airway Pressure machines connect to a face mask that cover the nose and mouth. It pumps pressurized air through the mask to keep the airway from collapsing. Patients sometimes struggle to use this mask every night as it can take some getting used to. They are not always particularly comfortable and can cause dry mouth. Some patients also report feeling claustrophobic.
- Oral Appliance – A less invasive but equally effective option is an oral appliance. These custom fitted mouthpieces move the jaw forward and prevent the soft palate from collapsing. Patients often report greater compliance with oral appliance than the CPAP because it is easier to use. Greater compliance with using your appliance helps to reduce your health risk factors and ensures you get better sleep.
In some cases it may be necessary to combine treatment options. At Sleep Better Columbus we dedicate ourselves to finding the best solutions for our sleep apnea patients. We tailor our sleep apnea therapy to each patient to address their individual needs and concerns. If you or someone you love suffers from sleep apnea, or feel may be suffering from it, please contact Dr. Levy for a screening consultation.
Is sleep apnea dangerous? Call Sleep Better Columbus at (614) 362-7292 to discuss your risk factors.